If you’re reading this after a crash, fall, or assault, and you don’t feel like yourself, you’re not “crazy.” You may be dealing with a traumatic brain injury (TBI) or concussion. TBIs are often invisible on the outside but very real in the brain and body. As a clinical psychologist, neuroscientist, and attorney, I see the same pattern again and again: symptoms are minimized, scans look “normal,” and people are told to tough it out. That’s not acceptable, and it’s not how the science works.
What a concussion/TBI actually is
- A concussion is a traumatically induced disruption of brain function. You don’t need a skull fracture or loss of consciousness.
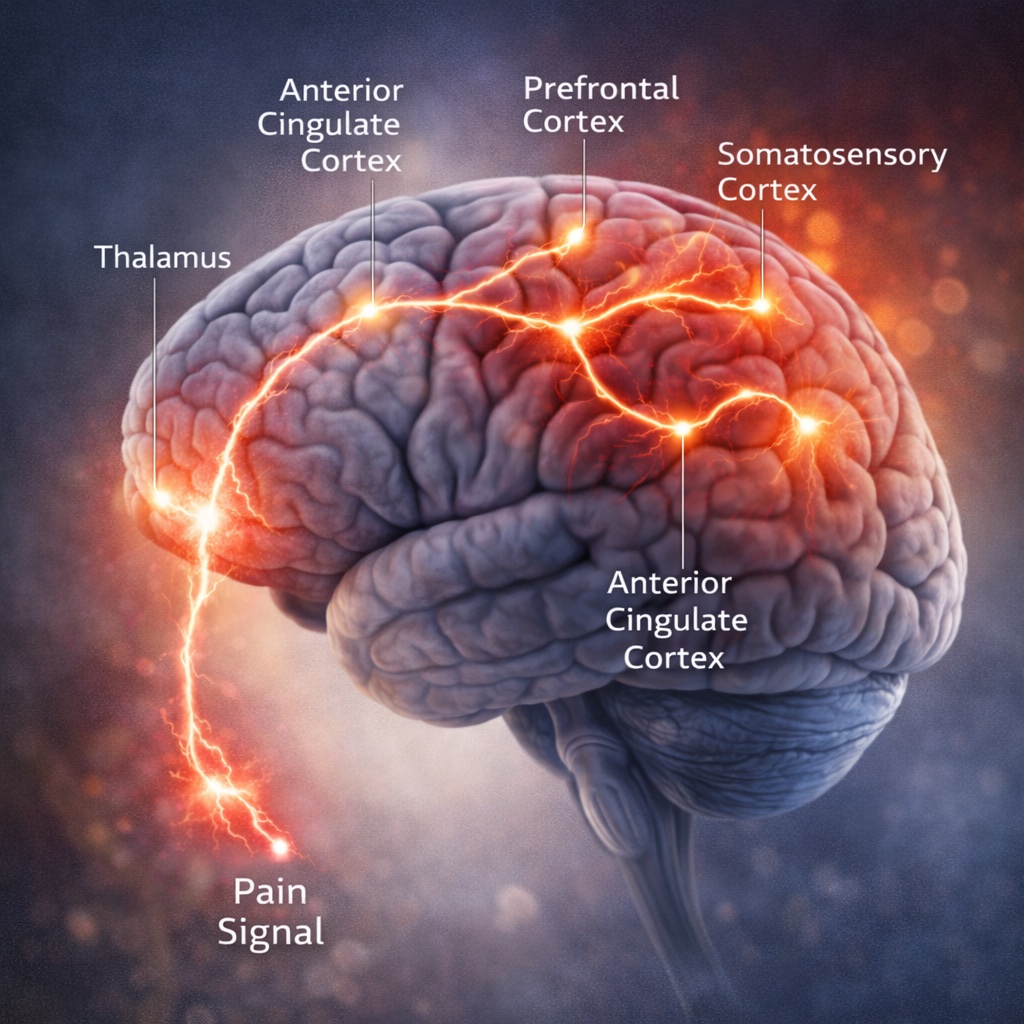
- The brain can be jolted, stretched, and temporarily disrupted at a cellular level. Think “wiring problem,” not “bruise you can see.”
Common, real symptoms
- Cognitive: slowed thinking, word-finding trouble, attention and memory lapses.
- Physical: headaches, dizziness, light/sound sensitivity, sleep disturbance, fatigue.
- Emotional/behavioral: irritability, anxiety, depression, short fuse, tearfulness.
- Overlap with PTSD: hypervigilance, insomnia, concentration problems, and irritability often occur in both TBI and PTSD, which is why clear evaluation matters.
Why your scan may be “normal” but you’re not
- Most mild TBIs do not show obvious damage on routine CT or MRI. That does not mean you weren’t injured. Courts have recognized that normal imaging doesn’t rule out a severe functional impact when symptoms and testing support TBI.
- Brain injuries are often substantiated by multiple data points: neurological exams, neuropsychological testing, symptom trajectories, medical records, collateral reports, and sometimes advanced imaging or physiological measures. This is the standard, credible way to prove an “invisible” injury.
TBI and PTSD often travel together
- After a traumatic event, the brain’s alarm system can stay stuck “on.” Both TBI and PTSD can produce sleep problems, concentration issues, irritability, and anxiety. Distinguishing them requires careful assessment, but for many people, both are present and both deserve treatment and compensation.
What to do in the first days and weeks
- Get evaluated early. Tell providers about head impact, whiplash, or any gap in memory.
- Track symptoms. A simple daily log of headaches, sleep, focus, mood, and triggers helps doctors treat and helps lawyers prove damages.
- Protect recovery. Prioritize sleep, hydrate, reduce overstimulation, and pace back to work/school with medical guidance.
- Watch for red flags. Worsening headaches, repeated vomiting, confusion, weakness, or slurred speech need urgent care.
How a trauma-informed lawyer builds your case A strong TBI case is evidence-driven and survivor-centered. Here’s what we do:
- Listen for the “before vs. after” story. Who you were pre-injury compared to who you are now matters. Family, coworkers, coaches, and friends help document the change.
- Assemble the right experts. Depending on your case, that can include neurologists, physiatrists, clinical neuropsychologists, vestibular therapists, and, when relevant, PTSD experts.
- Use the right testing. Neuropsychological assessments can objectively quantify attention, processing speed, memory, and executive function deficits, even when scans are normal.
- Document the overlap and the differences. If PTSD symptoms are present, we show how both conditions impact your life and earning capacity, and we push back on attempts to dismiss either as “just emotional.” The research supports that PTSD has physical, brain-based components too.
- Prove the future. We translate the medical picture into clear life-care, rehab, and vocational needs so insurers, judges, and juries understand the true cost of your injury.
Why choose a neuroscience-informed, trauma-informed firm Most firms try to move hundreds of files at once. We cap our active caseload at 25 so we can do the deep work your case requires. You’ll hear from us every two weeks, guaranteed. We lead your case and collaborate with top trial lawyers and medical experts when it benefits you. If we’re not the right fit, we’ll help you find someone who is.
When to call
- You hit your head or had whiplash and now feel “off.”
- Your CT/MRI was “normal,” but you can’t think, sleep, or function like before.
- You’re being told it’s “stress,” while people who know you see real changes.
- You’re months out and still symptomatic.
What you can expect from us
- A calm, clear intake focused on you, not just your paperwork.
- A plan to get the right evaluations.
- Consistent communication and rigorous, science-backed advocacy.
If an injury has changed your brain or your peace of mind, you deserve a team that understands both. Reach out. Even if you’re not sure you have a case, we’ll help you make a smart next step.



.jpg)
.jpg)