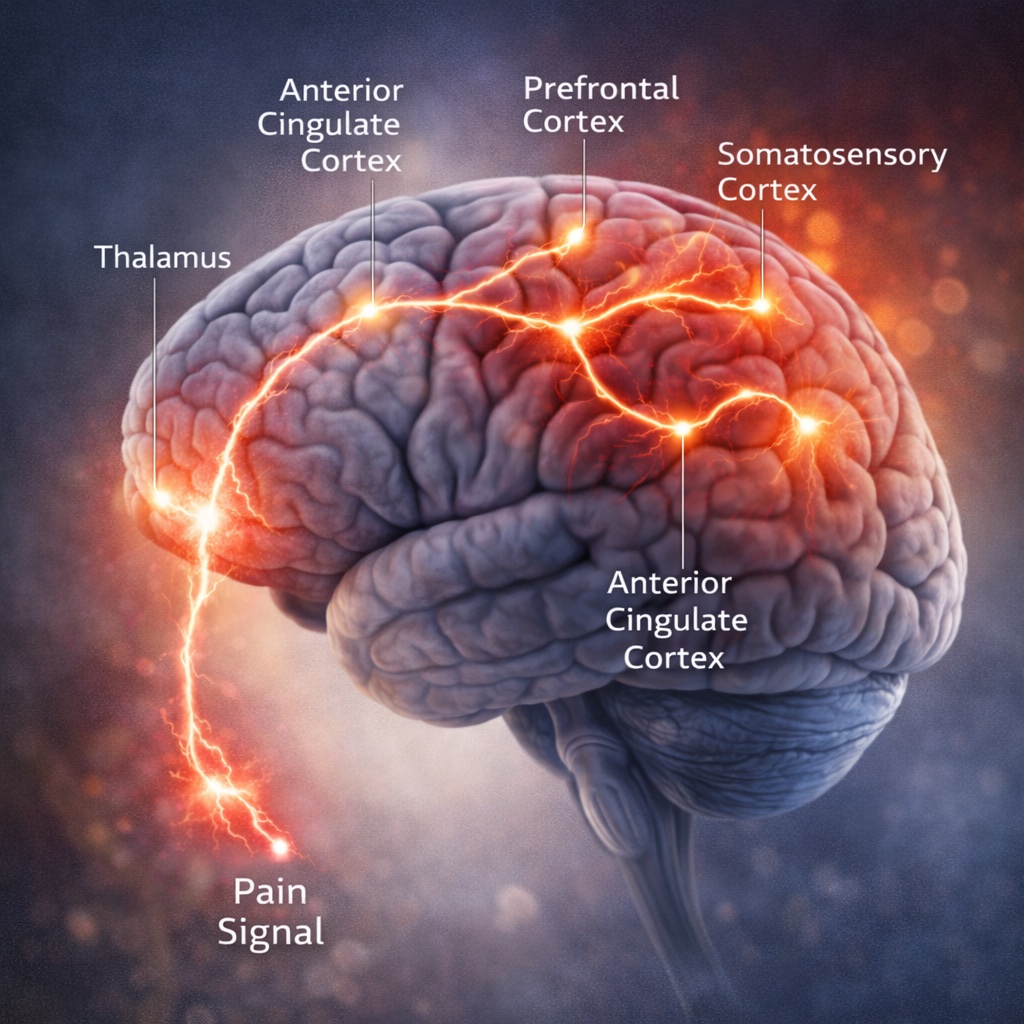
I want to reframe a phrase that’s often weaponized against survivors: “It’s all in your head.” When we’re talking about pain, physical or emotional, that statement is anatomically true. Pain is constructed by the brain using a distributed network that includes the anterior cingulate cortex (ACC), insula, thalamus, prefrontal cortex, amygdala, and brainstem modulators like the periaqueductal gray. In my trainings and slides I map this pain network and teach why experience, context, and meaning shape what we feel. The ACC helps predict and monitor pain, the insula computes intensity and bodily state, and the prefrontal cortex appraises and “tells the story” of what the signals mean. Pain is never “just nerves”; it’s perception plus interpretation across this system.
Here’s the key for legal cases: the brain uses much of the same circuitry for physical pain and emotional pain. In my law review article on PTSD as bodily injury, I discuss the classic Eisenberger and Lieberman work showing social exclusion activates many of the same regions involved in physical pain, especially the ACC and insula. Later research expanded this overlap and tied in prefrontal and limbic contributions. In plain language, heartbreak and a broken bone don’t feel identical, but the brain recruits a common alarm-and-meaning network for both. That’s why emotional injuries can ache, and why physical injuries carry an emotional sting.
What this means for PTSD
- PTSD isn’t a “soft” injury. It produces measurable brain and body changes and engages the same pain network that constructs physical suffering. Chronic amygdala threat signaling, altered prefrontal regulation, and insula disruptions help explain hyperarousal, avoidance, numbing, sleep disruption, and the sense of being on edge. These shifts show up in psychophysiology and, in some cases, imaging.
- The overlap with physical pain explains why symptoms can feel automatic and consuming. When the ACC expects harm, the insula amplifies intensity, and the prefrontal story skews toward danger, pain becomes louder—whether the trigger is a loud noise or a courtroom question.
Why “normal scans” don’t end the conversation Routine CT or MRI often miss functional changes that drive symptom burden. Strong cases don’t hinge on a single picture; they rest on converging evidence: careful medical and psychological evaluation, validated symptom measures, neuropsychological testing when indicated, psychophysiology, and sometimes targeted advanced imaging. The invisible becomes visible when we look with the right tools.
How we use this science in your case
- We translate your lived experience into brain-language decision-makers understand, using the pain network as the bridge. When a defense suggests your PTSD is “just emotional,” we explain, with evidence, that emotional pain recruits the same neural machinery that constructs physical pain. That is biology, not weakness.
- We document the “before and after” across thinking, sleep, startle, concentration, relationships, and work. Then we connect those changes to known brain systems so judges, juries, and insurers see why your symptoms persist and what it will take to treat them.
- If you also have a concussion or TBI, we make the map even clearer: where TBI contributes, where PTSD contributes, and how the shared pain circuitry magnifies impact. This blocks false either-or narratives.
What you can do now
- Get evaluated. Tell providers about the event, head/neck forces, memory gaps, and all symptoms, including “emotional” ones. Those are bodily, too.
- Track patterns. A brief daily log of sleep, headaches, anxiety spikes, triggers, and pacing helps clinicians treat and helps us prove damages.
- Seek trauma-informed care. It supports recovery and creates credible records that reflect how your brain and body were changed.
At Sweeton Injury Law, I’m your point person, and I collaborate with top medical and legal experts to build the kind of converging proof this science supports. We cap our caseload at 25 so you get real attention and biweekly check-ins. If we’re not the right fit, I’ll help you find a team who is.
Bottom line: If someone tells you it’s “all in your head,” the answer is yes! Because that’s where pain lives for all humans. In PTSD, that same network has been reshaped by trauma. The law should recognize that. We do, and we build your case accordingly.



.jpg)
.jpg)